Health Care Coverage and Enrollment During the Pandemic
Health Care Coverage and Enrollment During the Pandemic
At the beginning of the pandemic, unemployment rates in California, and nationally, soared when many businesses closed to shelter in place and mitigate the spread of the virus. With the rising unemployment rates during an unprecedented health crisis, there was a lot of uncertainty around accessing health care in 2020, including getting coverage for those who may have lost employer-sponsored coverage or their financial means. Throughout the ITUP 2020 workgroups, we discussed with our local partners the perplexing slower-than-expected rise in Medi-Cal enrollments during the pandemic and local challenges and best practices to ensuring health care coverage in communities across the state.
ITUP Links and Resources
ITUP 2020 Regional Fact Sheets
ITUP 2021 Regional Fact Sheets
ITUP Policy Forum: Where are All the People?
Perplexingly Low Medi-Cal Enrollment in the First Year of the Pandemic
Where are all the people? This was a common question that came up in all of our workgroups when we asked participants about the status of health care coverage of their communities. It was so common, in fact, that ITUP used this question as the title for a Fall 2020 Enrollment Policy Forum that highlighted workgroup participants’ on-the-ground experiences for our statewide policy audience. Estimates based on trends experienced during the 2008 recession predicted significant increases in enrollment in publicly-funded coverage programs, including Medi-Cal and Covered California. However, as shown in the chart below, only slower and more moderate enrollment increases were observed. This was especially true among highly impacted groups.
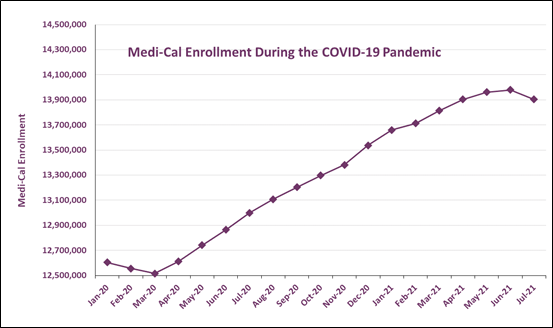
Source: Department of Health Care Services, Medi-Cal Certified Eligibles Tables, by County from 2010 to Most Reportable Month, Accessed: September 12,2021.
Workgroup participants thought that slower enrollment was due to a variety of factors that we discuss below. They include:
- Fear of public charge;
- Delayed employment layoffs;
- Employers maintaining health coverage for furloughed or laid-off employees;
- Delays in uninsured people seeking routine medical care for conditions other than COVID-19; and,
- Lack of information about, familiarity with, and stigma of health care coverage provided by the government (such as Medi-Cal and Covered California).
Best Practices and Challenges for Getting and Keeping People Covered Throughout the COVID-19 Pandemic
Local Best Practices
- Expanded Access to Coverage and Services for Uninsured and Vulnerable Californians. From the beginning of the pandemic in early 2020, many Californians faced financial stress and loss of employment. As a result of the economic impacts, early in the pandemic and around the time that ITUP held the Regional Workgroups, the state Department of Finance predicted that the pandemic would result in a 2 million person increase in Medi-Cal enrollment. At this time, many workgroup participants discussed coverage options made temporarily available because of the pandemic as a best practice for keeping people covered. Since in-person Medi-Cal enrollment was not safe during the COVID-19 pandemic, participants in several regions reported that trusted and flexible enrollment options were implemented to ensure stable access to Medi-Cal. Examples of ways local partners met the coverage and enrollment needs in their communities include:
- DHCS suspended Medi-Cal redetermination for the remainder of the pandemic’s public health emergency;
- Both commercial and public health insurers were required to provide coverage for COVID-19 testing and treatment;
- Uninsured people being treated in hospitals for COVID-19 were granted “presumptive eligibility” for Medi-Cal, ensuring that people were covered for their hospital costs and allowing hospitals providing care to uninsured patients to be paid;
- Mendocino and San Diego regions reported implementing a variety of options for remote enrollment, including zoom and curbside assistance for those without access to the internet;
- Promatores and other community health workers were essential for outreach and help navigating health insurance enrollment, including addressing digital literacy and language barrier needs of their communities; and,
- Humboldt and North Central region participants discussed additional coverage options such as the Path to Health program for undocumented Californians to access primary care and prescription medications. Since these workgroups were held, Governor Newsom signed the FY 2021-22 state budget which included funding to expand health insurance access to undocumented Californian’s ages 50 years and older. Undocumented adults between the ages of 26-49 still remain ineligible for full-scope Medi-Cal coverage.
Local Challenges
- Economic Fallout Create Challenges in Coverage and the Delivery of Health Care. At the onset of the pandemic, unemployment numbers climbed rapidly, hitting their peak at 16 percent in April 2020. With many Californians facing major financial straits and sudden change and uncertainty in employment, enrollment in public programs, such as Medi-Cal, were expected to rise.
- In several workgroups, health care coverage was impacted by:
- County political landscapes;
- Wildfires;
- Fear of the safety of health care workers due to personal protective equipment shortages;
- Care needs that were not previously identified; and,
- Financial constraints, including small business employees falling through the cracks and not knowing their options for coverage and enrollment.
- In several workgroups, health care coverage was impacted by:
Shift in Public Outreach Capacity and Process. Limited outreach at the onset of the pandemic was identified by participants from several regions as a significant challenge to enrolling Californians in coverage. It was suggested that many of those thrown into unemployment may not know how to enroll in government-sponsored health insurance, including Medi-Cal and Covered California (See ITUP’s Health Insurance Coverage Options During COVID-19 Fact Sheet). Additionally, the lack of physical, in-person outreach and enrollment efforts in very rural, isolated regions, migrant farmworker communities, and in schools was also a barrier.
- Stigma Around Medi-Cal, Covered California, and Trust Issues Towards the Government. Participants reported that stigma and trust issues, including public charge, as mentioned above, were notable barriers to coverage for many Californians.
- Combatting the belief or stereotype that Medi-Cal coverage provides lower quality care than marketplace or commercial plans;
- Consumers who have lost their jobs waiting for their employment to return before seeking health insurance; and,
- Immigrant communities prefer to apply for coverage in-person because of distrust of the system.
- Fear of Public Charge. Public Charge was the common thread running through workgroup discussions across the state on coverage and enrollments during COVID-19. While the Trump Administration’s Public Charge guidance is no longer in effect as of March 9, 2021, participants from the Central Valley, Orange County, Mendocino, and the North Central regions all identified Public Charge as a major barrier to health care access during ITUP’s 2020 workgroups.
- It was reported that some people in the North Central region who qualified for Medi-Cal were concerned about Public Charge and believed enrolling in Medi-Cal would eventually be used against them.
- Participants in the Central Valley and Humboldt regions shared that they heard from members asking for their Medi-Cal accounts to be closed due to Public Charge concerns.
- Despite Public Charge fears from many workgroup participants, in Orange County, Medi-Cal enrollments in the Asian American and Pacific Islander community still occurred. The Medi-Cal enrollment outcomes in Orange County were attributed to the work of community-based organizations (CBOs) utilizing community health workers and other stakeholders who committed time and resources to outreach and education in these communities. When it came to COVID-19 testing and California’s Presumptive Eligibility Program, however, hesitation still exists in AAPI communities.
- Despite effective education, the same Orange County participant noted that health care access barriers related to immigration are not limited to Public Charge. They discussed how the assault on immigrants has been relentless the last three years and while clients may not understand all the nuances to policies, they understand it is safer to go underground instead.
Next Steps
ITUP continues to follow these issues and connect with our local partners around health coverage enrollment. As the pandemic continues, and California begins to recover from the crisis, the policies initiated by the public health emergency will inevitably be lifted. During the pandemic, the federal government suspended redeterminations for Medi-Cal enrollment, meaning that once an individual was enrolled in Medi-Cal after March 2020, they remained covered and enrolled. Because this is a temporary policy, California is preparing for those Medi-Cal redeterminations and for many people to no longer have Medi-Cal coverage. Initially, states would have six months after the public health emergency was declared over to complete redeterminations and verifications for Medi-Cal members, however, the Center for Medicare and Medicaid Services (CMS) has extended this to allow states twelve months post public health emergency. There will be a great need to ensure that individuals and their families receive assistance in applying for and enrolling in other health care coverage options, including Covered California and employer-sponsored/job-based commercial health insurance.
To receive updates from the Department of Health Care Services (DHCS) on the Medi-Cal program, including changes to coverage, you can subscribe to receive stakeholder updates here.
Stay tuned for more ITUP blogs highlighting state level policies, budget updates, and more insights from our local partners!





